Understanding Gynecological Conditions & Disorders of the Breast for Veterans
For many women veterans, gynecological conditions and disorders of the breast can significantly impact their health, daily life, and overall well-being. These conditions can arise or be exacerbated by military service due to factors like stress, environmental exposures, military sexual trauma (MST), or direct injuries. Whether it’s chronic pelvic pain, fertility issues, hormonal imbalances, or breast-related concerns, these conditions can lead to discomfort, functional limitations, and long-term health challenges.
Securing VA disability service-connection for these conditions hinges on comprehensive and precise medical documentation. The VA evaluates these conditions under specific criteria outlined in 38 CFR Part 4, Subpart B, Diagnostic Codes 7600-7632 (for gynecological conditions and disorders of the breast).
Essential Medical Evidence for Gynecological Conditions
Let’s explore the essential medical evidence needed for some of the most common gynecological and breast conditions that affect women veterans.
Endometriosis
Endometriosis is a chronic condition where tissue similar to the lining of the uterus grows outside the uterus, causing pain, inflammation, and potential fertility issues.
Essential Medical Evidence:
- Gynecologist or specialist evaluation clearly diagnosing endometriosis.
- Surgical reports (e.g., laparoscopy findings) confirming the presence and extent of endometrial implants.
- Detailed symptom documentation: Severity and frequency of pelvic pain, dysmenorrhea (painful periods), dyspareunia (painful intercourse), fatigue, and gastrointestinal symptoms.
- Impact on daily life: Documentation of missed work/school, limitations on physical activity, social withdrawal, or interference with relationships.
- Treatment history: Records of hormonal therapies, pain management, surgeries, and their effectiveness or side effects.
Uterine Fibroids (Leiomyomas)
Non-cancerous growths of the uterus that can cause heavy bleeding, pelvic pain, pressure, and reproductive issues.
Essential Medical Evidence:
- Gynecologist diagnosis supported by imaging (e.g., ultrasound, MRI) detailing size, number, and location of fibroids.
- Symptom documentation: Severity and frequency of heavy menstrual bleeding (menorrhagia), pelvic pain/pressure, frequent urination, or painful intercourse.
- Anemia documentation: If caused by heavy bleeding, include CBC results showing low hemoglobin and iron studies.
- Treatment records: Details of medical management (e.g., medications, hormonal therapy) or surgical interventions (e.g., myomectomy, hysterectomy), including post-surgical complications and residual symptoms.
- Functional impact: Documented limitations in physical activity, energy levels, and occupational performance due to symptoms.
Your symptoms, fully documented.
Schedule your consultation with our medical evidence experts today.
Polycystic Ovary Syndrome (PCOS)
A hormonal disorder common among women of reproductive age, often characterized by irregular periods, excess androgen levels, and polycystic ovaries.
Essential Medical Evidence:
- Endocrinologist or gynecologist diagnosis based on Rotterdam criteria (two of three: irregular periods, signs of high androgens, polycystic ovaries on ultrasound).
- Lab results: Documented elevated androgen levels (e.g., testosterone), abnormal glucose tolerance, insulin resistance.
- Ultrasound reports showing polycystic ovaries.
- Symptom documentation: Details on irregular or absent periods, hirsutism, acne, weight gain, hair loss, and fatigue.
- Related conditions: Documentation of associated conditions like type 2 diabetes, cardiovascular issues, or mental health impacts (depression, anxiety).
- Treatment history: Records of medications (e.g., metformin, birth control pills) and their effectiveness.
Menstrual Disorders (e.g., Amenorrhea, Dysmenorrhea, Menorrhagia)
Abnormalities in the menstrual cycle, including absent periods (amenorrhea), severe pain (dysmenorrhea), or excessively heavy/prolonged bleeding (menorrhagia), especially if service-connected or exacerbated.
Essential Medical Evidence:
- Gynecologist diagnosis specifying the type of menstrual disorder.
- Detailed menstrual history: Duration, frequency, severity of bleeding, and associated pain.
- Symptom impact: Documentation of how pain, heavy bleeding, or fatigue affects daily activities, work attendance, and quality of life.
- Lab tests: CBC if anemia is suspected due to heavy bleeding.
- Treatment records: Medications, hormonal therapies, or procedures (e.g., D&C, endometrial ablation) and their outcomes.
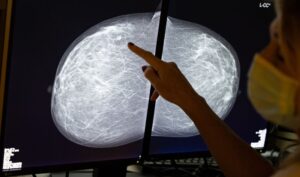
Breast Cancer
Malignant tumors originating in the breast tissue, a serious condition requiring extensive documentation of diagnosis, treatment, and residual effects.
Essential Medical Evidence:
- Oncologist diagnosis with detailed pathology reports (biopsy, surgical pathology) specifying cancer type, stage, grade, and receptor status.
- Imaging reports: Mammograms, ultrasounds, MRIs, and PET/CT scans documenting tumor size, lymph node involvement, and metastasis.
- Treatment records: Comprehensive documentation of chemotherapy, radiation therapy, surgery (e.g., lumpectomy, mastectomy), hormone therapy, and targeted therapy, including dates, cycles, dosages, and side effects.
- Residual symptoms/complications: Documentation of pain, fatigue, neuropathy, lymphedema (include circumference measurements), disfigurement, range of motion limitations post-surgery/radiation, and mental health impacts.
- Post-treatment status: Clear records indicating remission, recurrence, or ongoing treatment.
Benign Breast Conditions (e.g., Fibrocystic Changes, Cysts)
Non-cancerous breast conditions that can cause pain, tenderness, and lumps, potentially requiring ongoing monitoring or intervention.
Essential Medical Evidence:
- Breast specialist or gynecologist diagnosis supported by clinical examination and imaging (mammogram, ultrasound, MRI).
- Pathology reports confirming benign nature (if biopsy performed).
- Symptom documentation: Severity, frequency, and location of breast pain, tenderness, or presence of lumps/cysts.
- Functional impact: Documentation of how pain or discomfort affects daily activities, sleep, or ability to wear certain clothing.
- Treatment/management records: Details of pain management, aspiration of cysts, or ongoing monitoring.

Documenting Secondary Conditions Associated with Gynecological & Breast Issues
Gynecological conditions and breast disorders can often lead to or worsen other medical issues. Thorough documentation is vital to establish these important secondary service connections:
Due to Chronic Gynecological Pain (e.g., from Endometriosis, Fibroids):
- Chronic Pelvic Pain Syndrome: Detailed pain management notes, physical therapy records, and specialist evaluations confirming persistent, debilitating pain.
- Mental Health Conditions: Therapist or psychiatrist records documenting anxiety, depression, or PTSD directly linked to chronic pain, fertility struggles, or the impact on intimacy and relationships.
- Fatigue: Medical documentation of chronic fatigue impacting daily functioning and directly related to ongoing pain or heavy bleeding.
- Gastrointestinal Issues: Records linking chronic pelvic inflammation or pressure to symptoms like IBS, constipation, or urinary frequency.
Due to Breast Cancer & Its Treatment:
- Lymphedema: Objective measurements of limb circumference (post-mastectomy/lymph node dissection), physical therapy notes documenting swelling, pain, and functional limitations.
- Neuropathy: Neurologist evaluations detailing nerve damage (e.g., from chemotherapy, radiation), its severity, and impact on sensation/function.
- Chronic Pain: Documentation of persistent pain at surgical sites, from radiation, or due to nerve damage.
- Fatigue: Oncologist/medical records noting severe, treatment-induced chronic fatigue.
- Mental Health: Therapist/psychiatrist records documenting depression, anxiety, or body image issues related to diagnosis, treatment, or disfigurement.
- Thyroid Dysfunction: Lab results and endocrinologist notes linking thyroid issues to radiation therapy.
- Cardiovascular Conditions: Documentation of heart issues (e.g., cardiomyopathy) as a long-term side effect of specific chemotherapy agents or radiation.
Examples of Documentation: Weak vs. Strong
Example 1: Endometriosis
- Weak Example: “Patient reports pelvic pain. Has endometriosis. Takes pain meds.”
- Strong Example: “Patient diagnosed with Stage III Endometriosis (ICD-10: N80.3) via laparoscopic surgery on 10/15/2023, confirming extensive peritoneal implants and adhesions. Patient reports daily severe pelvic pain (rated 8/10), debilitating dysmenorrhea requiring bed rest for 3-5 days per cycle, and dyspareunia limiting intimacy. Pain is poorly controlled despite continuous oral contraceptives and NSAIDs. Functional limitations include frequent absenteeism from work (averaging 4 days/month), inability to participate in previously enjoyed physical activities, and significant impact on social and marital relationships due to chronic pain and fatigue. Patient reports exacerbation of symptoms since active duty service began in 2010 with onset of severe menstrual irregularities.”
Example 2: Breast Cancer (Post-Treatment)
- Weak Example: “Veteran had breast cancer. Finished treatment. Follow-ups ongoing.”
- Strong Example: “Veteran diagnosed with Invasive Ductal Carcinoma, Stage II (ICD-10: C50.911), ER/PR+, HER2- via biopsy 03/2022. Underwent lumpectomy 04/2022 followed by chemotherapy (AC+T regimen, 6 cycles completed 09/2022) and radiation therapy (25 fractions completed 11/2022). Residual symptoms include Grade 2 peripheral neuropathy in bilateral feet confirmed by neurologist (EMG 01/2023), causing chronic numbness and gait instability. Reports severe, persistent fatigue (rated 9/10) impacting all ADLs and limiting work to part-time capacity. Diagnosed with Grade 2 lymphedema of the right arm (circumference difference 3.5 cm at forearm), requiring daily compression garment use and lymphatic drainage therapy, severely impacting right arm strength and function, preventing lifting >5 lbs.”
Essential Diagnostic Tests & Documentation
Comprehensive documentation requires clearly detailed results from lab tests, imaging studies, and physical assessments:
- Gynecological Conditions:
- Laparoscopy and hysteroscopy operative reports (endometriosis, fibroids)
- Ultrasounds/MRIs offering clear imaging evidence
- CA-125 where relevant, complete hormonal panels, CBC for anemia
- Breast Conditions:
- Mammograms, breast ultrasounds, MRI and detailed biopsy/pathology results
- Imaging clearly demonstrating the location, size, nature (benign vs. malignant)
- Lymphedema objective measurements clearly documented (in cm)
- Functional impairments noted with range of motion limitations numerically

Questions to Ask Your Healthcare Provider
Ensuring thorough, detailed medical documentation requires proactive discussion:
- “Could you document detailed objective findings (such as measurements, clinical scales) clearly in my medical records?”
- “Please explicitly document how this condition impacts my daily life and functional capabilities.”
- “Could you provide detailed documentation of all treatments and therapies including response to these interventions?”
Essential Medical Documentation Strategies
- Regularly schedule provider visits to keep consistent clinical documentation.
- Maintain symptom journals to accurately track condition fluctuations, treatments, and outcomes for supporting evidence.
- Be specific with your healthcare providers regarding how your condition impacts your daily tasks, occupation, family, and social interactions.
- Ensure complete documentation of your prescribed treatments, medication response, procedures, and secondary symptoms or conditions clearly stated by your provider.
The VA offers special programs to support the welfare, health, and dignity of female veterans and their families. Visit Women Veterans Health Care to discover the health care and services you have earned as a woman veteran.
Disclaimer
This guide provides educational insights on medical documentation of gynecological conditions and breast disorders. It does not constitute medical, legal, or benefit-specific advice. For personalized medical guidance, always consult qualified healthcare professionals.